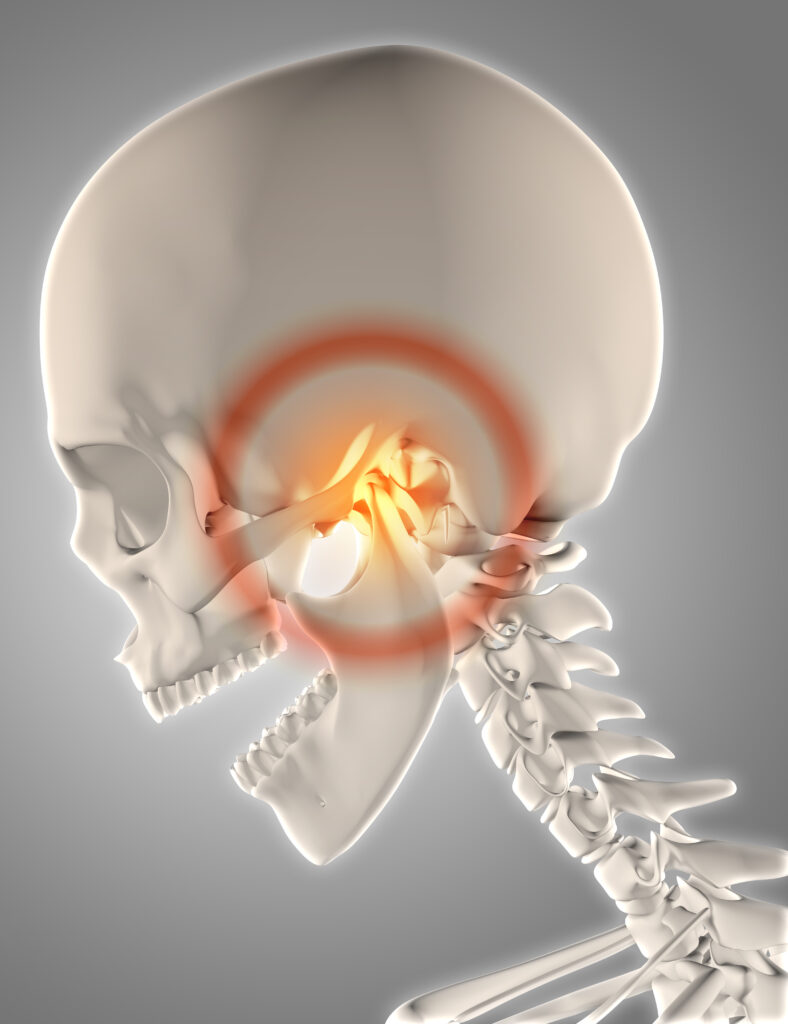
Temporomandibular disorders (TMDs) are problems with the muscles and joints that connect your jaw to your skull. The disorders cause pain when you talk, chew, swallow, or yawn. You may feel this pain on one or both sides.
The temporomandibular joint disorder is a term that includes a group of painful and dysfunctional conditions that involve the muscles of mastication and the TMJ, so it’s a nonspecific term that covers a wide variety of painful jaw conditions.
TMJ disorders may be the result of 2 main causes —-
- An abnormal muscular function, or
- Degenerative changes within the joint.
What is a TMJ disorder?
- Joint pain at rest or during function.
- Painful clicking.
- Dysfunction (chewing difficulties, jaw deviation, jaw locking, etc.).
- Sudden unexplained bite changes.
TMJ disorder is defined by pain either at rest or upon function.
It is defined by something that is a painful noise.
It can also be just dysfunction like a limited range of motion or a jaw deviation such as when you open you go to one side or you are unable to go from one side to the other or sudden unexplained bite change like you wake up and your jaw is to the front, or to the side. Those are considered TMJ disorders. They can be associated with headaches and ear pain.
The temporomandibular joint commonly referred to as TMJ is a pair of joints where the mandible lower jaw meets the temporal bone base of the skull just forward of the ears. Since it is a pair of joints, the right and left sides must function together in harmony.
This is a very complex joint as a matter of fact the temporomandibular joint is the most complex joint in the body. It is the only joint in the human body to have a rigid endpoint of closure which is where the teeth make contact to limit jaw movement. It is also a compound joint, a joint involving at least three bones in the body; the mandible, the temporal bone and the articular disk.
You can imagine the strain that we place on this joint as we breathe, talk, eat, and swallow 2000 times per day. It is no wonder that 34% of the population reports some level of disorder in the TMJ. The normal movement of this joint is both a rotation and a sliding motion. As we begin to open our mouths the rotation aspect of movement begins and as we continue to open the mouth the lower jaw actually begins to slide downward and forward. The basic components of this joint consist of bone, tissue, muscle, ligaments, tendons, and a disc which acts like a small pillow or cushion protecting the joint from where sort of like a shock absorber.
The temporomandibular joint disorder is characterized by signs and symptoms including pain in the area of the TMJ or the surrounding muscles which often limits the mandibular range of motion. TMD is typically caused by various types of trauma when the disc remains in its proper position during normal opening and closing of the jaw no clicking or popping should occur. If the joint makes noise when opening and closing it is due to friction within the joint.
SYMPTOMS OF TMJ DISORDER:
- Pain or tenderness of your jaw.
- Pain in one or both of the temporomandibular joints.
- Aching pain in and around your ear.
- Difficulty chewing or pain while chewing.
- Aching facial pain.
- Locking of the joint makes it difficult to open or close your mouth.
- Pain in the face and jaw.
- Jaw locking.
- Clicking, popping, or grinding sounds
- Sensitive teeth facial pain that worsens when the person uses their jaw.
- Joint and muscle tenderness.
- Limited range of motion.
- Jaw alignment issues.
- Ringing in the ears.
- Earaches.
- Headaches with or without ear pain and pressure behind the eyes.
- Toothache.
TYPES OF TMJ DISORDER:
- Muscle.
- Joint.
- Systemic disease.
We classify them as TMJ disorders involving the muscles of mastication, involving the joint itself, or part of systemic disease.
1. MUSCLE DISORDERS:
- Guarding
- Spasm
- Myositis
- Myofascial pain
- Fibrosis
- Tendinitis
The muscle disorders are for the TMJ and the muscles of mastication are just exactly the same as for any muscles in your body. There is muscle ache, restriction of range of motion, fibrosis, and tendinitis.
MUSCLES OF MASTICATION:
- Masseter
- Temporalis
- Medial pterygoid
- Lateral pterygoid
Muscles of mastication are usually for the most part the masseter and temporalis muscles. Those are the ones that give people the most trouble.
2. JOINT DISORDERS:
We can have a joint disorder that is directly associated with a disc dysfunction. It is held by ligaments and it goes forward and backward, so there are a lot of possibilities for things to go wrong as far as this little disc.
3. SYSTEMIC DISEASE:
- Arthritis
- Rheumatoid arthritis
- Lupus.
- Tumors of the jaw
CAUSE OF TMJ DISORDER:
TMDs are often caused by tight jaw muscles. The tightness can be caused by clenching or grinding your teeth. This may happen when you have a lot of stress in your life. If you lower your stress, you may be able to stop clenching or grinding your teeth. This will help relax your jaw and reduce your pain. Your doctor may suggest a dental splint. Splints can help reduce teeth grinding and clenching. You may also be able to do some things at home to feel better. But if none of this works, your doctor may prescribe medicine to help relax your muscles and control the pain.
Causes of articular disorder:
- Noninflammatory arthropathies.
- Inflammatory arthropathies.
- Growth disturbances.
- Neoplasms.
- Diffuse connective tissue disorders.
Causes of non-articular disorder:
- Muscular disorders.
- Growth disturbances.
- Neoplasms.
Several adverse conditions occur in TMD situations.
The open lock is when the condyle and disc move too far forward and get caught over the anterior slope of the imminence of the temporal bone. This is an open lock and will cause the patient to have difficulty closing his mouth. Disc displacement with reduction is caused by trauma that is damaged or stretched the ligaments causing the disc to be out of position too far forward concerning the head of the condyle as the mouth begins to open the disk is in front of the condyle. As the condyle slides downward and forward, the condyle pops back into position on top of the disk. This causes a popping or clicking sound when closing the mouth the disc remains in its proper position and then just before the condyle returns to its position of origin the condyle slips off the disk and another popping sound occurs. This second sound may be softer and not as noticeable.
Disc displacement without reduction is when the posterior ligaments have been severely stretched or torn. These are the ligaments that hold the disc on the head of the condyle. If this occurs the disc remains in front of the condyle throughout the entire opening and closing process. Most TMD patients worsen with time. Slight clicking advances to more frequent clicking and eventually to jaw locking as the posterior ligaments continue to stretch allowing the disc to move further and further out of position. When the disc has slipped too far forward or inward, the jaw will lock shut often referred to as a closed lock an acute closed lock occurring usually due to trauma is a situation in which there is an audible noise or pop as the disc slips out of place and the person cannot open their mouth.
The chronic closed lock is a problem that persists for more than 6 months. The disc is never positioned between the bones and the opening and closing cycle. During this time, the disc will degenerate and lose its shape. The patient may begin to open wider and wider as the disc is slowly destroyed. Pain and arthritis will set in due to bone-on-bone rubbing. Depending on the severity of the problem there are several treatment options available to treat TMD.
What is NOT a TMJ disorder?
- Clicking without pain or dysfunction.
- Popping without pain or dysfunction.
- Crepitus without pain or dysfunction.
- Radiographic changes in the joint without active DJD.
If there is no pain, no dysfunction, if you are able to open your mouth wide, if you are able to chew without pain, you don’t have a TMJ disorder. You may have noises, you may have joint noises, but you do not have, by definition, a TMJ disorder. You can have abnormal findings in an MRI or an x-ray without having a TMJ disorder. There are a lot of people and certainly, most of us over 40 will have some type of changes on an x-ray, even though we are still completely asymptomatic and we can chew and we can open our mouths without any restrictions. That is a kind of something that comes up a lot. There are patients who come in because they have joint noises and because they have been told by their dentist that they had a TMJ disorder or because the dentist saw on the x-ray that there was something abnormal. So, of course, we can determine it. But, as a rule of thumb, if you don’t have any pain or dysfunction, you don’t have a TMJ disorder and you don’t have to worry. About 60% of people pop and click, so it is a very common incidence. They don’t really consider it a disorder because it’s a variation of normal at this point.
TREATMENT OF TMJ DISORDERS:
First line:
- NSAIDs
- Corticosteroids
- Physical therapy
- Trigger point injection
- Joint manipulations
Adjunct:
- Meditation
- MBSR
- Splint therapy
- Moist heat/ice
- Muscle relaxants
- Pain psyche (counseling, medications)
Rarely:
- Surgery
Never:
- Orthodontics
- Bite adjustments
- Opioids
All the treatments that are done for TMJ disorder are reversible. So things like full-time wear of splints can change your bite in a permanent way. So if you wear a splint day in and day out for several months, your bite will most likely change and what you do at that point that you need braces some people actually have a phase one and phase two process where they change the bite on purpose with the use of a full-time appliance and then afterward they restore the bite to a better position. So, stay away from treatments that are not reversible.
Splint therapy consists of the placement of removable or fixed dental appliances which protect or keep in place the injured body part. The purpose of this type of therapy is to reduce inflammation and pain. This type of therapy will not restore all of the damaged or degenerated components.
Orthotic therapy is similar to splint therapy, however, an orthotic is used to support, align, prevent or correct deformities or improve the function of movable parts of the body. The goal of orthotic therapy is to provide the best condyle fossa relationship possible, to decompress the joint which reduces inflammation, and to restore correct muscle length bilaterally.
Surgery is only recommended in about 2% of TMD cases as with all medical treatment diagnosis is key your physician or dentist may refer you to a doctor either an MD or dentist who has received extra training in the diagnosis and treatment of TMD you will undergo testing to determine the cause and extent of dysfunction and be given treatment options comprehensive treatment may include referral to other professionals such as chiropractors, naturopaths, physical therapists, massage therapist or podiatrist to provide you with whole body care to address your condition.
How can you care for yourself at home?
- Put either an ice pack or a warm, moist cloth on your jaw for 15 minutes several times a day. You can try switching back and forth between moist heat and cold.
- Make eating easy on your jaw. Choose softer foods that are easy to chew like eggs, yogurt, or soup. Avoid hard foods that cause your jaws to work very hard. Try cutting your food into small pieces. And if your jaw gets too painful to chew, or if it locks, you may need to puree your food for a while.
- To relax your jaw, repeat this exercise for a few minutes every morning and evening. Watch yourself in a mirror. Gently open and close your mouth. Move your jaw straight up and down. But don’t do this if it makes your pain worse.
- Manage stress. You may be clenching or tightening your muscles when you are under stress.
- Get at least 30 minutes of exercise on most days of the week to relieve stress. Walking is a good choice.
- Ask your doctor if you can take over-the-counter pain medicine, such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin), or naproxen (Aleve). Be safe with medicines. Read and follow all instructions.
- Use good posture for sitting and standing. Slumping your shoulders disturbs the alignment of your facial bones and muscles.
- Don’t:
- DON’T hold a phone between your shoulder and your jaw.
- DON’T open your mouth all the way, like when you sing loudly or yawn.
- DON’T clench or grind your teeth, bite your lips, or chew your fingernails.
- DON’T clench things such as pens, pipes, or cigars between your teeth.
When should you call for help?
Call your doctor or seek immediate medical care if:
- Your jaw is locked open or shut or it is hard to move your jaw.
- Your jaw pain gets worse.
- Your face is swollen.
- You do not get better as expected.
THANK YOU
MEDICAL ADVICE DISCLAIMER:
This blog including information, content, references, and opinions is for informational purposes only.
The Author does not provide any medical advice on this platform.
Viewing, accessing, or reading this blog does not establish any doctor-patient relationship.
The information provided in this blog does not replace the services and opinions of a qualified medical professional who examines you and then prescribes medicines.
And if you have any questions of medical nature, please refer to your doctor or qualified medical personnel for evaluation and management at a clinic/hospital near you.
The content provided in this blog represents the Author’s own interpretation of research articles.
